Editor’s note: The Federal Motor Carrier Safety Administration has submitted a Notice of Proposed Rulemaking that would regulate testing and treatment of truck drivers and other transportation workers suffering from sleep apnea. The proposal is expected to be published in the Federal Register in January, 2016. With this proposal in mind, we asked sleep apnea expert Michael Decker about current research and treatment options for this disease.
Michael Decker, PhD, Registered Nurse, Registered Respiratory Therapist and Diplomate of the American Board of Sleep Medicine is Associate Professor in the School of Nursing at The Frances Payne Bolton School of Nursing at Case Western Reserve University. His work with sleep apnea began in 1986 at Case Western Reserve's pulmonary research laboratory directed by Kingman Strohl. It was one of the first centers in the country that was a Specialized Center of Organized Research, SCOR; their specialty was sleep and sleep apnea. Decker understands sleep issues as well as trucking. Before entering medicine, Decker was a truck diesel mechanic and body repairman. He has family members and friends who are in the trucking industry.
In layman's terms, what is sleep apnea?
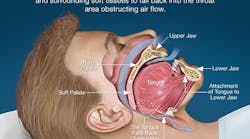
Sleep apnea is a disorder in which the upper airway muscles do not work properly during sleep and the upper airway collapses. When the upper airway collapses, the amount of oxygen in a person’s bloodstream falls rapidly. Levels of carbon dioxide increase rapidly, and this and other changes lead to an arousal from sleep.
What causes the airway to collapse?
This is what a lot of people don’t understand. Sleep apnea is an inherited disorder. We think of it as much like a neuromuscular disease of the upper airway. The part of the brain that controls the upper airway fails to work properly in people who have sleep apnea. And their upper airway doesn’t work well when they’re awake, too. They simply have less strength in their upper airway muscles. Many people have sleep apnea but the disease may not show itself unless there’s a trigger. That trigger, for instance, can be a change in weight or alcohol use. That trigger can be a broken nose making it difficult to breathe. Sleep apnea is a genetically-conferred disorder that may or may not show itself until a certain triggers occurs.
If a trucker has sleep apnea there’s a one-in-four chance that some of his children have it. Kids with sleep apnea have reduced academic performance. They don’t do well in school. They can become hyperactive. I often encourage a person who may have sleep apnea to get tested. Even if you may not want treatment yourself, your children may have this disorder, and they need treatment because it’s going to impact the rest of their life.
How do people know if they suffer from sleep apnea?
Sleep apnea occurs during sleep and many people are unaware that they have it. I believe a general statistic is that 80 to 90 percent of people with sleep apnea are unaware that they have the disease. The symptoms and signs of sleep apnea are daytime sleepiness, depression, changes in mood or behavior. These are all behaviors or traits that people often attribute to age or working too hard. The symptoms of sleep apnea are very general, so it makes it difficult for the afflicted person to know if they have the disease. It’s usually their bed partner who tells them that they have it, or there is an event where they fall asleep during driving or at work.
How is sleep apnea diagnosed?
Sleep apnea can only be diagnosed with systems that monitor breathing and blood oxygen levels during sleep. You cannot diagnose sleep apnea with a questionnaire. You cannot diagnose sleep apnea sitting in a doctor’s office. There can be a high suspicion, but the diagnosis has to be done with a sleep monitoring device.
A monitoring device, especially portable sleep systems, have little bands that go around the chest. There's also one device called a finger oximeter that attaches to your finger like a clothespin and it measures blood oxygen levels. People can pick these up in the doctor’s office and take it home and wear it at night. Some doctors, however, prefer that their patients go into a sleep laboratory, where they can monitor brain activity in addition to breathing activity and oxygen levels.
What are the long term effects of sleep apnea?
My main focus has been understanding how low levels of oxygen that occur during a sleep apnea event lead to changes in brain chemistry and how those changes impact daytime performance and vigilance. Preliminary results by us and others show that the low oxygen induced by sleep apnea leads to long-term changes in the brain dopamine system and another part of the brain called the hippocampus, which is involved with memory. There are recent studies published this year [2015] that show there are changes in white matter across the brain, and white matter is the axonal pathways that connect one part of the brain to another. There’s a substantial amount of preclinical and clinical research showing brain changes that are sleep apnea induced.
These are not healthy changes, and it’s unclear if they are reversible.
Some truck drivers have reported receiving a CPAP machine without going into a sleep lab or having their vital signs monitored. Is that good medicine?
If we have a driver who reports, “My wife says I'm choking during the night. I'm not breathing. I can’t stay awake while driving,” then you’re going to preemptively treat that person with a CPAP because CPAP works instantaneously. Is it worth putting that person and others around them at risk for six weeks on the road while a sleep study is scheduled, or do you go ahead and treat them right away and say you know this isn’t going to be perfect but it’s going to make you feel a lot better and keep you alert and possibly alive until we get you into the laboratory? The answer often is 'yes.'
Is CPAP the only treatment for sleep apnea?
No. There are others. It’s very difficult for people to adapt to CPAP because it's blowing air into your face; it’s like having a vacuum cleaner running in reverse connected to a mask attached to your face. It’s very difficult to breathe against that. So many people are just unable to tolerate CPAP. They make an honest effort but they’re just not able to adapt to that high pressure in their face.
There are things like oral appliances and there are neurostimulators that work well. There is a new device called Inspire which is like a heart pacemaker. It is a neurostimulator that gets implanted right below the collarbone for example. There is a little wire that runs up to the muscles of the neck. When the person sleeps, this stimulator applies a little electrical pulse to the nerve that controls the upper airway, and that pulse keeps the upper airway open. Remember that said sleep apnea is caused by s a neuromuscular problem, and there is no electrical drive to the muscles of the upper airway. This pacemaker restores that drive and keeps the airway open. It was approved by the Food and Drug Administration in 2014. You turn it on when you go to sleep, perhaps by passing a little magnet over your chest and that turns it on. They’re very effective. The secret is picking the right patient, because there are certain people it won’t work in and other for whom it works exceptionally well.
What has been your professional experience with truck drivers and sleep apnea?
Before I came to Case Western I was in Georgia and I owned my own clinical sleep center. One of the things that I learned is that many truck drivers come into a sleep center under an assumed name and pay cash because they know they are sick and want to be treated; they want to be safe. That taught me more than anything that people know when they’re sick and they want to be treated, but they’re always worried about the retribution of losing their job.
Is there anything else you would like truck drivers to know about sleep apnea?
Sleep apnea is important but there are many other disorders that are more prevalent that can cause the same amount of daytime sleepiness. For example, there is restless leg syndrome/periodic limb movement in sleep. I was not a big believer in this until I trained at Emery. I trained in the Department of Neurology and I would see people who couldn’t stay awake at work. They were falling asleep on their desk, and they had periodic limb movement. It's a disorder of the autonomic system. So in restless legs syndrome, it’s not the person’s leg that twitches; that’s an unfortunate name. What happens is that the brain sends a signal to the spinal cord. The person’s blood pressure shoots up. Their heart rate shoots up. They have an autonomic discharge, and their leg just coincidentally twitches as part of this. That was the outward sign that we noticed. When this whole event occurs, the person’s sleep transitions just like in sleep apnea. They move from deep sleep to light sleep so it causes an arousal, and this can happen with the same frequency as breathing problems in sleep apnea. They have all the same problems with depression and vigilance. Periodic limb movement disorder may be as high as 15 percent in the population. It tends to be overlooked, yet the consequences can be just as severe.
What's your main message to truck drivers with sleep apnea?
My key message is that with treatment sleep apnea is reversible, and people can have an absolutely happy normal life with it. They just have to reach out and get help.